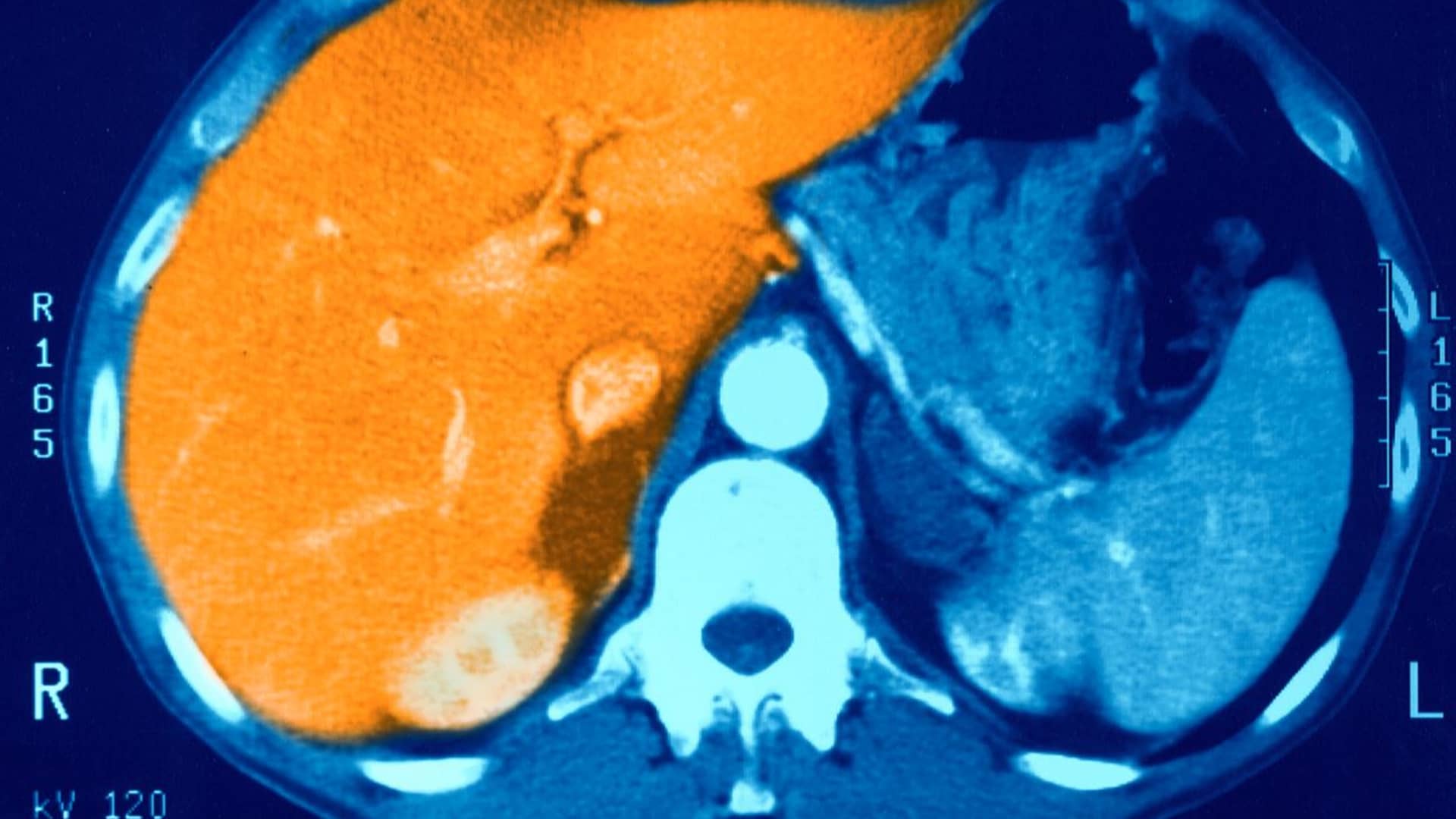
Image of a healthy liver not ravaged by fatty liver disease.
BSIP | Getty Images
Think a friend or colleague should be getting this newsletter? Share this link with them to sign up.
Good afternoon! Drugmakers aren’t just racing to develop drugs that treat obesity. They’re also competing to expand the uses of those weight loss treatments, including for a severe form of liver disease.
Some drugmakers – including the dominant players in the market, Novo Nordisk and Eli Lilly – have already demonstrated the drugs’ ability to help patients shed unwanted pounds and regulate blood sugar.
Now, they aim to show the treatments can bring additional health benefits. Doing so could unlock even more revenue from the booming market, and expand the limited insurance coverage for those treatments, most of which cost close to $1,000 per month.
The competition heated up on Monday after Denmark-based drugmaker Zealand Pharma and its partner Boehringer Ingelheim posted strong results from a mid-stage trial testing its drug, survodutide, in patients with metabolic dysfunction-associated steatohepatitis, or MASH. That condition is characterized by excess fat buildup and inflammation in the liver and can lead to liver scarring, or fibrosis.
Survodutide, which helped overweight patients or those with obesity lose up to 19% of their weight in another phase 2 trial, is just one of a long list of drugs that could eventually become treatments for MASH.
An update to STAT’s obesity drug tracker on Monday shows that at least 23 – or about one-fifth – of the 105 weight loss drugs in development or on the market are also being investigated for their ability to treat the condition.
So, why are drugmakers focusing on this specific form of liver disease? For one, there are no medicines approved to directly target MASH. The drugs being tested may not cure the condition, but their reach could be large: Around 115 million people worldwide are affected by MASH, and an estimated 3% to 5% of U.S. adults have the condition, according to some studies.
The new data underscores the potential for weight loss drugs to help. Up to 83% of trial participants treated with survodutide saw significant improvements in their disease with no worsening of liver scarring after 48 weeks, compared with 18.2% in a group who received a placebo, according to Zealand Pharma.
Survodutide also met one of the second aims of the trial, which was showing a “statistically significant” improvement in liver scarring. There were also no unexpected safety or tolerability issues among those who received the drug, even at higher doses.
Riley Securities analyst Mayank Mamtani said the data “materially surpassed investor expectations,” and even appears to improve upon mid-stage trial data that Eli Lilly released earlier this month.
Around 74% of patients who received the highest dose of Eli Lilly’s drug, tirzepatide, became free of MASH with no worsening of liver scarring after a year. That compares with around 13% of those who received a placebo.
It was less clear how much that drug reduced liver scarring, which was the second aim of the trial. Eli Lilly did not disclose whether tirzepatide met that goal, but the company said the drug’s effect on decreasing scarring was “clinically meaningful” across all dose sizes.
However, Jefferies analysts cautioned in a Monday note that Eli Lilly’s trial included patients with more severe forms of liver scarring compared to Zealand Pharma’s study. That may explain the differences in data.
The two drugs work differently. Zealand Pharma’s treatment mimics a gut hormone called GLP-1, which suppresses appetite, but it also imitates another hormone called glucagon. Meanwhile, Lilly’s tirzepatide targets GLP-1 and a different hormone called GIP.
It’s too early to say whether one drug is better than another at treating MASH. It will likely take years before we see Eli Lilly and Zealand Pharma’s drugs on the market as a fatty liver disease therapy.
Boehringer Ingelheim told Reuters on Monday that the company hopes survodutide will launch as a treatment for MASH or obesity in 2027 or 2028, contingent on favorable trial data.
Full results from both Eli Lilly and Zealand Pharma’s mid-stage trials will be presented at a medical conference this year. We also have to wait for data from other drugmakers: Novo Nordisk is studying semaglutide, also known as Wegovy for weight loss and Ozempic for diabetes, in a late-stage trial for treating MASH.
But one biotech company may be the first to bring a successful MASH drug to market: The Food and Drug Administration is slated to decide whether to approve a medication called resmetirom from Madrigal Pharmaceuticals on March 14.
Latest in health-care technology
Change Healthcare outage rolls into seventh day after cyberattack
Traders work at the post where UnitedHealth Group is traded on the floor of the New York Stock Exchange.
Brendan McDermid | Reuters
It’s been a rough week for Change Healthcare.
The company, which offers solutions for payment and revenue cycle management, said its systems are down for a seventh straight day after parent company UnitedHealth Group disclosed that a “suspected nation-state associated” cybersecurity threat actor gained access to part of its information technology network last week.
The extent and nature of the breach remains unknown, but UnitedHealth said it isolated and disconnected the affected systems “immediately upon detection” of the threat, according to a filing with the U.S. Securities and Exchange Commission on Thursday.
The company did not disclose exactly what Change Healthcare systems the attack disrupted, but the breach has caused problems across health systems and pharmacies at companies like CVS Health and Walgreens.
UnitedHealth told CNBC late Monday that more than 90% of all U.S. pharmacies have set up modified electronic claims processing workarounds to mitigate the impact of the outage, while the remaining pharmacies have set up solutions offline.
For consumers like Cary Brazeman, the disruption has been a headache.
Brazerman tried to pick up a prescription at a Vons pharmacy in Palm Springs, Calif., on Saturday, but he was told that the pharmacy hadn’t received the transmission from his doctor. Even if the location had, employees said they wouldn’t have been able to run his insurance.
“I’m like, ‘OK, what am I supposed to do now?’ and they’re like, ‘We don’t know,'” Brazerman told CNBC in an interview.
By Monday, Brazerman said the pharmacy had set up a workaround that helped it communicate with some insurance companies, but not all. He said he is planning to go back to his doctor to pick up a paper copy of his prescription, bring it back to the pharmacy and hope for the best.
His immediate concern is not if his information was compromised, he said, but whether the people who really need medication can access it. Especially patients who have conditions more serious than his own.
“I’m mobile, so I can make these rounds if necessary, and I can pay cash if necessary, but there’s a lot of people who cannot,” he said.
Feel free to send any tips, suggestions, story ideas and data to Annika at annikakim.constantino@nbcuni.com and Ashley at ashley.capoot@nbcuni.com